CE Certified COVID-19 Test Now Available
April 30, 2020
From MAY 1st 2020 VirQ SARS-CoV-2 Fast One-Step PCR Test for the Detection of COVID-19 has been CE certified.
Unlike most assays on the market, it is able to exclude false negative results caused by lack of cell material taken during sample collection.
This multiplex-PCR with 3 colour detection is compatible with most common thermalcyclers

January 17, 2019
MC Diagnostics are delighted to announce that our Quality Management System has been certified to ISO 13485:2016 by the leading UK Based EU Medical Body, BSI.
What is ISO 13485:2016? ISO 13485 is a stand-alone, international quality standard which supports Medical Device manufacturers to implement Quality Management Systems, that establishes and maintains effectiveness to their processes. Specifically, ensuring consistent design, development, production and delivery of Medical Devices that are safe and to their intended purpose.
What does this mean for our customers? By obtaining this quality standard accreditation, this demonstrates MC Diagnostics true understanding of the requirements and highlights our commitment to conduct high-level quality control, product traceability, risk-management and the importance of meeting customer and regulatory requirements. Overall, giving our customers peace of mind that our products are designed, manufactured and delivered to a high-standard but also, that we are in ful

August 7, 2018
Haemovigilance is an important aspect of transfusion science concerning the minimization of adverse effects and adverse events. One of the more serious complications following a blood transfusion is a haemolytic transfusion reaction, where donor blood contains antibodies incompatible with patient blood. The adverse event occurs when red blood cells given during the transfusion are destroyed by the recipient’s immune system.
July 29, 2018
Coeliac disease is a T-cell-mediated chronic autoimmune disease which effects the absorption of nutrients in the small intestine due to surface inflammation. The symptoms are caused by disease-specific antibodies against endomysium or tissue transglutaminase, which inflict damage to the lining of the intestine upon ingestion of gluten. Commonly reported symptoms include stomach pain and cramping, nausea, ongoing fatigue, constipation, diarrhoea, weight loss, mouth ulcers and bloating. Around 1 in 100 people has coeliac disease although this can be easily misdiagnosed for other GI problems. Early diagnosis is critical, as the intake of gluten can have destructive effects on the small intestine causing malabsorption, malnutrition, lactose intolerance which can cause health complications including osteoporosis, iron deficiency anemia, vitamin B12 deficiency and bowel cancer. Coeliac susceptibility is associated with the DQA1*05:01- DQB1*02:01 (DQ2) and DQA1*03-DQB1*03:02 (DQ8) haplotype and is dominantly inherited. Additionally, DR3, DR7 and DR11 alleles can be used as genetic markers. Of patients with coeliac disease, 99.6% of those will carry DQ8 or DQ2 [1]. HLA-DQ genotyping can be useful in accompanying a clinical disease diagnosis and to evaluate the risk of disease in relatives of a patient. To effectively treat coeliac disease a strict gluten-free diet must be followed, helping the intestines heal - which should lead to complete resolution of symptoms and decrease the risk of complications from long term malabsorption. Click here to find out more about our SSP and SSO kits used for coeliac testing.
1. Karell K, et al. Hum Immunol 2003; Apr;64(4):469-77
July 11, 2018
Polymerase chain reaction (PCR) is a highly sensitive technique to amplify a single copy of DNA into millions to billions of copies of a targeted sequence. Whilst its sensitivity is advantageous it can also create a number of issues if the correct contamination control is not followed. During PCR, even the smallest amount of contaminating DNA can be amplified resulting in the wrong template amplification and causing false positive or ambiguous results. Contamination can arise from work surfaces, equipment or reagents which have been exposed to PCR products. To minimize the risk of contamination there are several preventative methods and aseptic techniques which must be carefully performed.
June 7, 2018
Clinical laboratory measurements can be used for disease diagnosis, to guide pharmaceutical therapy, monitor disease progression and assess risk of recurrence. As an integral part of this, test procedure standardisation is essential to produce verifiable results, referring to the ability of an assay methodology to produce results which are both repeatable and reproducible. Inconsistent test procedures can lead to inconsistent assessment of a patient and, in some situations, incorrect diagnosis or treatment.
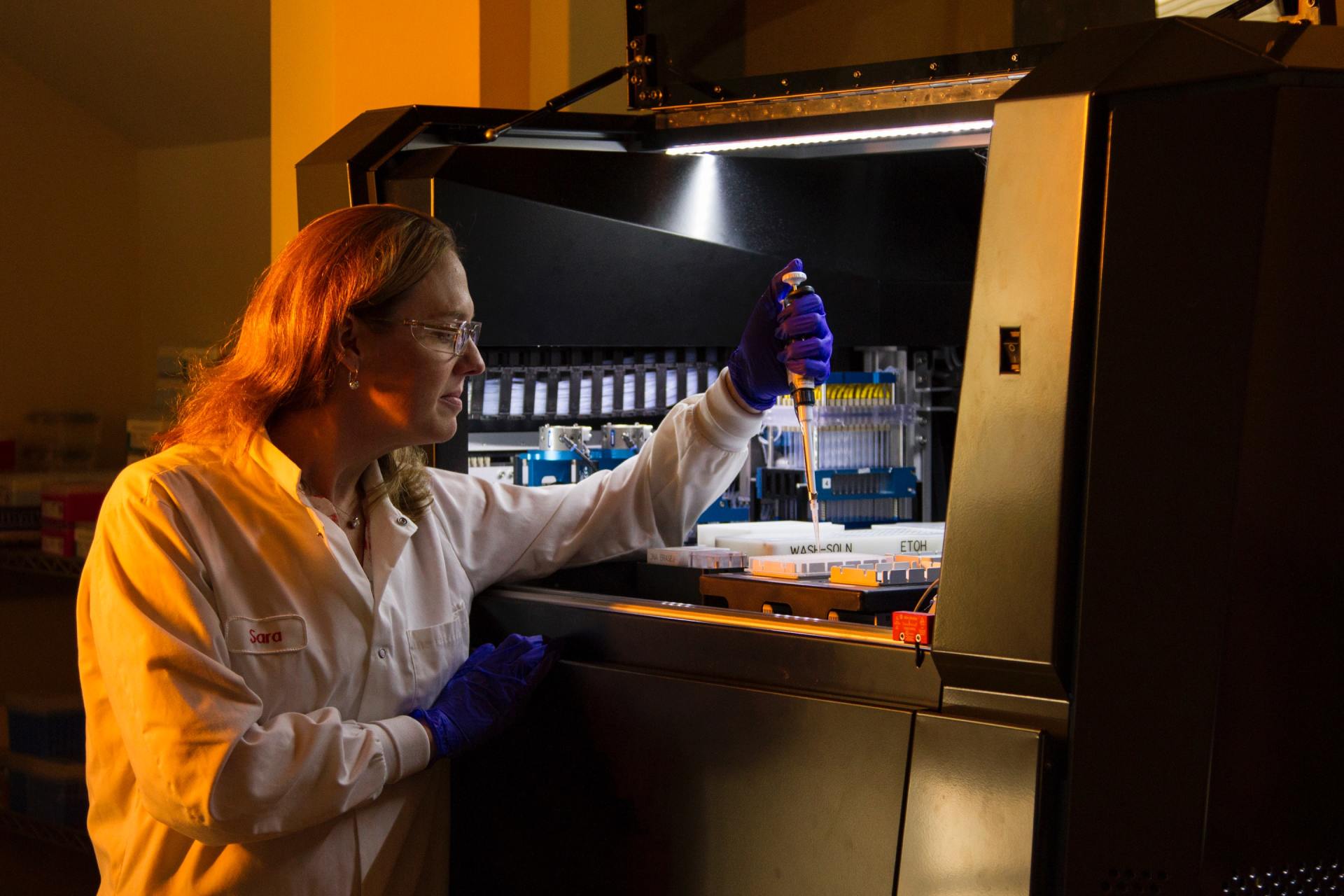
A barrier which assay standardisation faces is the consequence of manual handling errors on test variability. Many of the issues with consistency can be considerably reduced with the removal or reduction of human error by manual handling using automated assay technology.
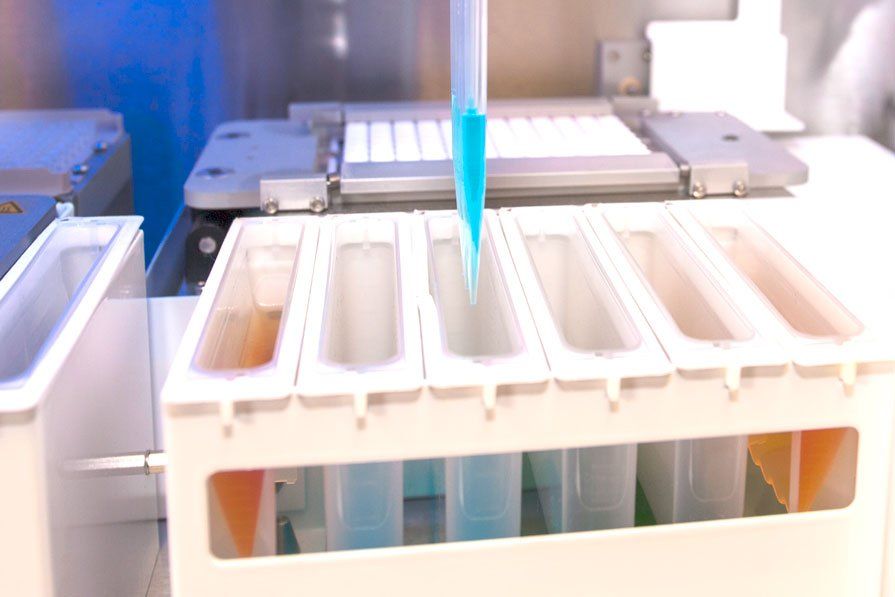
The ALDAS technology provides a complete platform to deliver simple, rapid, fully automated molecular diagnostics, that can easily be applied to a variety of application fields including immunogenetics, immunology, blood banking and microbiology. MCD has designed and developed the 3 elements of the system and can offer a tailored solution to meet your individual assay requirements.
The ALDAS instrument allows the complete automation of your assay by performing all hybridisation, pipetting and wash steps. The resulting reactivity pattern is visualised using colorimetric detection and an image captured by the on-board camera. The image is then transferred to our interpretation software for results analysis. PCR based assays can also be fully automated by the addition of a thermalcycler integrated into the instrument.
For more information about how our technology could improve your laboratory workflow click here to enquire
Versatility, Consistency, Reproducibility

June 6, 2018
Bechterew’s disease or Ankylosing Spondylitis is a chronic autoimmune disease effecting sacroiliac joints, spine, and peripheral arthritis. The incidence of disease generally occurs during teenage years and is three times more prevalent in males than females (3:1 ratio) (1). Common symptoms of Ankylosing Spondylitis include back pain and joint swelling, stiffness and extreme fatigue. The HLA-B*27 protein is a variant of the human leukocyte antigen-B (HLA-B) and has a strong association with this autoimmune disease and is therefore, used as part of the diagnostic procedure (2, 3). A positive HLA-B*27 result is associated with a very high disease risk. In suspected cases of Ankylosing Spondylitis, a HLA-B*27 diagnosis provides an important contribution to the therapy of the patient. Around 3% to 6% of the people carrying the HLA-B*27 gene develop Anklylosing Spondylitis and more than 90% of all patients with a seronegative arthritis have this gene.
From April 2018 our new HISTO TYPE B*27 realtime PCR kit for fast and easy detection of HLA-B*27 is available. The HISTO TYPE B*27 Q kit covers all common HLA-B*27 sub types. Moreover, the kit differentiates between the disease associated alleles and the sub types HLA-B*27:06 or HLAB*27:09, which are not associated with Ankylosing spondylitis (4). An easily implementable test compatible with most common realtime cyclers.Visit our technical page for further information on how this test is applied. 1. Braun, J et al., 1998. Arthritis & Rheumatism, 41(1), 58-67 2. Brewerton, DA et al., 1973. Lancet i:904-907
3. Schlosstien L et al., 1973. N. Engl. J. Med. 288:704-706 4. Kahn, MA et al., 2007. Autoimmunity Reviews 6: 183–189

May 4, 2018
The 32nd European Immunogenetics and Histocompatibility Conference (EFI) will be held in Venice, Italy from 9th to 12th of May, 2018. The BAG healthcare Lunch-Symposium will take place on Friday, May 11th from 12:00 to 13:00h on the third floor of Palazzo del Casinò, Sala Mosaici1. “First experiences with the HISTO SPOT HLA AB test for automated antibody diagnostics” John Smith PhD, FRCPath HCS Consultant Head of Tissue Typing Service Heart Science Centre Harefield Hospital Harefield, UK "Evaluation of the HISTO SPOT HLA AB test in comparison to a Luminex SA Test” Ing. Murielle Verboom Medizinische Hochschule Hannover Institute for Transfusion Medicine Transplantation Immunology Hannover, Germany
Secure Online Payments
Satisfaction Guarantee
International Service
Premium Customer Service
Inclusive Kits
Customer Chat
Copyright © 2024 MC Diagnostics Ltd.
All Rights Reserved.
Registered in England & Wales
Company Number: 5843597.
Tel: +44 (0)151 2039898
MC Diagnostics Ltd
1 Hawkshead Road
Croft Business Park
Bromborough
Wirral
CH62 3RJ
United Kingdom