Haemolytic Reactions In Blood Transfusion
Haemovigilance is an important aspect of transfusion science concerning the minimization of adverse effects and adverse events. One of the more serious complications following a blood transfusion is a haemolytic transfusion reaction, where donor blood contains antibodies incompatible with patient blood. The adverse event occurs when red blood cells given during the transfusion are destroyed by the recipient’s immune system.
Acute haemolytic transfusion reactions (AHTRs) occur shortly after a transfusion and is typically a result of an ABO incompatible transfusion. Delayed haemolytic transfusion reactions (DHTRs) occur more than 24 hours after transfusion in a patient who has previously been alloimmunised to a red cell antigen by blood transfusion or pregnancy. The antibody may have fallen to a level that is undetectable by the pre-transfusion antibody screen and the patient is then inadvertently re-exposed to red cells of the immunising group. Antibodies to the Kidd (Jk) blood group system are the most common cause of DHTRs reported to the MHRA via the Serious Hazards of Transfusion network (SHOT), followed by antibodies to Rh (D) antigens.
Haemolytic transfusion can cause major morbidity (requiring intensive care or renal dialysis) which occurs in up to 30% of cases and 5–10% of episodes contribute to the death of the patient. DHTRs caused 21.7% of transfusion related deaths in the UK between 2010 and 2016 with 35 cases of DHTRs in 2015-16 which possibly could have been avoided with better practice and diagnostic technology (SHOT annual report, 2016).
Blood banks routinely type blood donors and patients for ABO and Rh(D) as these are the most significant antigens to ensure a safe transfusion. The common (Kell, Kidd, Duffy, MNS) and rare blood group systems (Colton, Diego, Dombrock, Lutheran, Vel, KEL*3/4, KEL*6/7) and partial or weak-D alleles are not routinely typed for, but recipient plasma will be screened prior to transfusion for antibodies against rare antigens. If a patient has a positive cross match for a rare antibody or are transfusion-dependant they must receive blood units which lack the antigen(s) - necessitating the need for red cell phenotyping of the donor units.
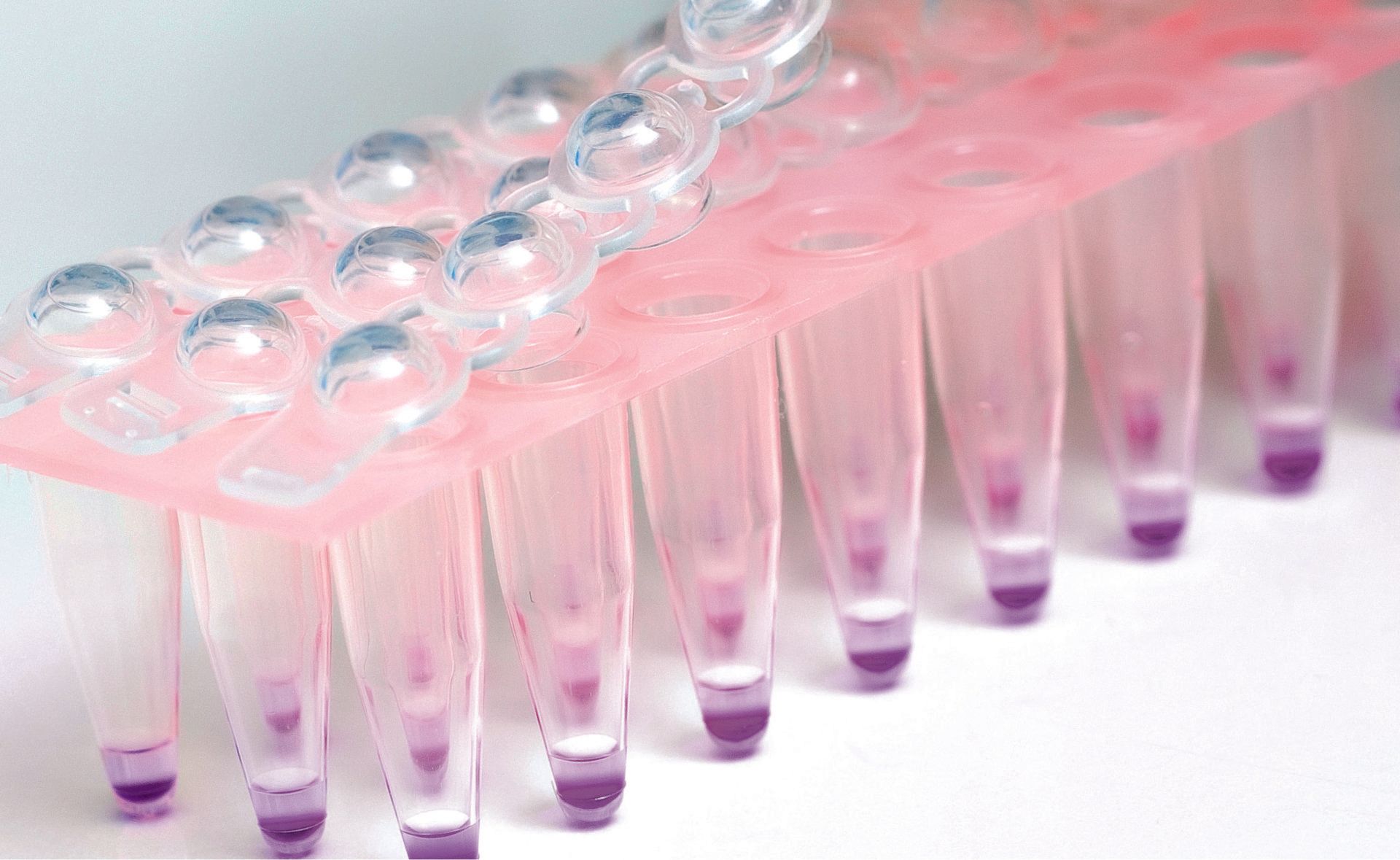
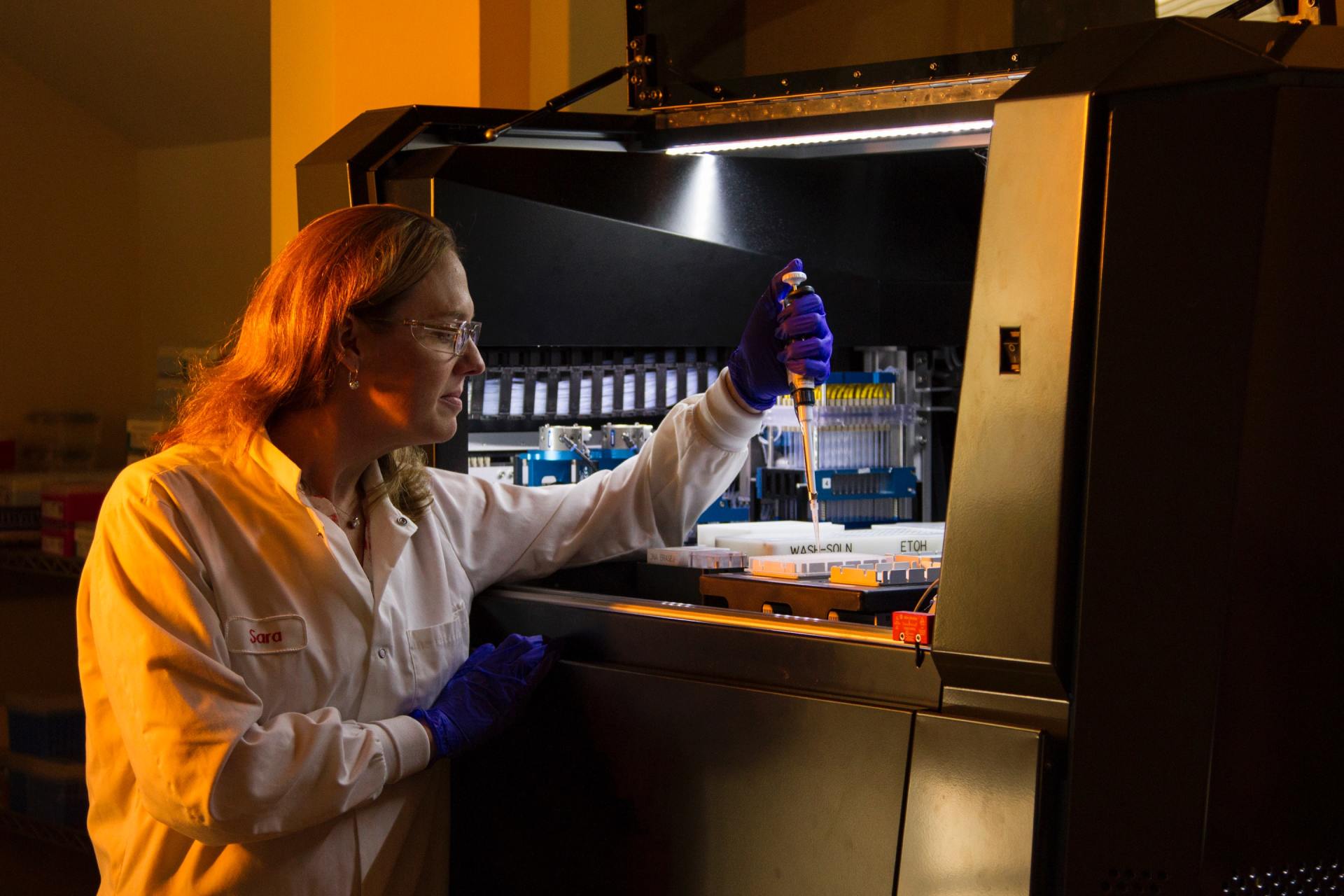
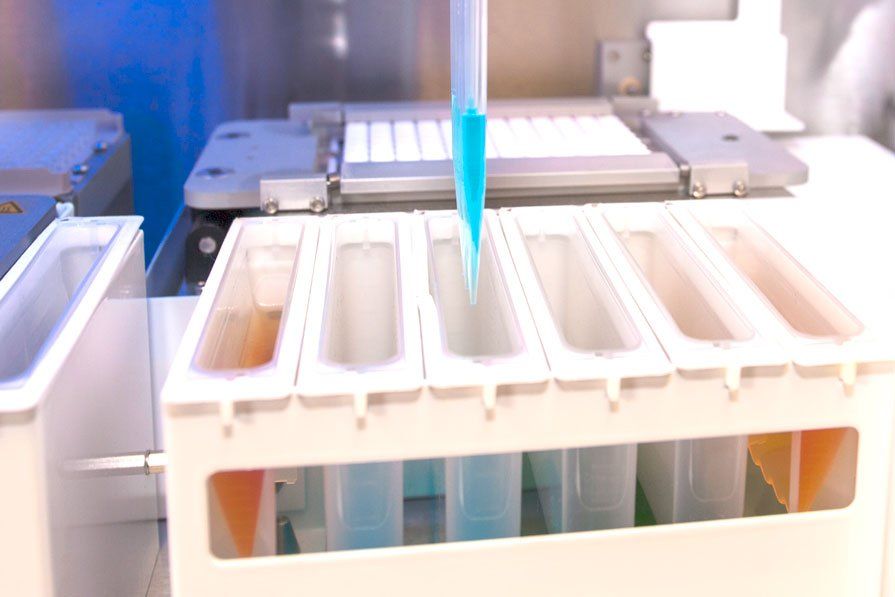
The conventional method for preventing DHTRs is serological typing, which uses antisera to detect antigen presence on red cells. Although this method is simple, it requires reliable antisera which can reaches its limits when it comes to the determination of rare blood group characteristics. Molecular blood group typing can provide a qualitative and selective result to better genotype patients phenotypical antigen characteristics. Molecular blood group typing enables a safe on-demand supply of blood preservations for patients with antibodies against clinically relevant, weak or rare blood group antigen specificities.
The molecular determination of blood group characteristics can be applied to on-demand situations and also used for pre-typing of blood donors. Pre-typing of blood donors has the advantage of increasing patient safety by preventing alloimmunisation, which in turn increases cost-effectiveness. In addition, due to its molecular based technology it works independently of antisera for rare antigens, which are often difficult to obtain and suboptimal in quality. For more information about our molecular blood group typing products - click here.