Molecular Contamination Control
Polymerase chain reaction (PCR) is a highly sensitive technique to amplify a single copy of DNA into millions to billions of copies of a targeted sequence. Whilst its sensitivity is advantageous it can also create a number of issues if the correct contamination control is not followed. During PCR, even the smallest amount of contaminating DNA can be amplified resulting in the wrong template amplification and causing false positive or ambiguous results. Contamination can arise from work surfaces, equipment or reagents which have been exposed to PCR products. To minimize the risk of contamination there are several preventative methods and aseptic techniques which must be carefully performed.
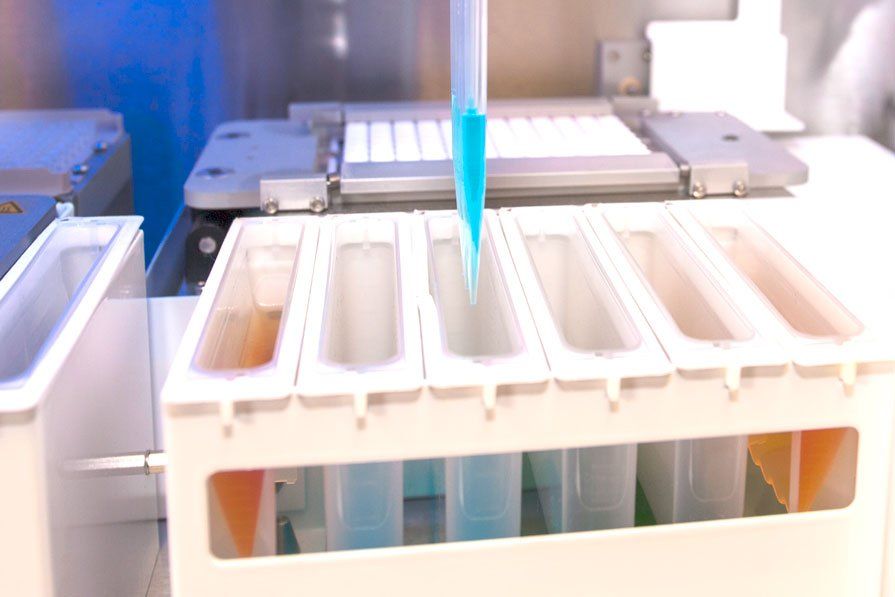
Establishing a unidirectional workflow and physically separating amplification setup pre-PCR from post-PCR is optimal to reduce the risk of contamination. Ideally PCR preparation and amplification should be physically separated or at least substantially separated within the same lab. Samples and reagents used in PCR setup should be in a different lab to the amplicon. This includes equipment and materials used for amplifying samples, such as thermal cyclers and instruments used for analysis (e.g. ALDAS & MR. SPOT processors). Each area should have its own designated equipment, including consumables and PPE to prevent cross-contamination occurring. The workflow should also continue in one direction: pre- to post-PCR, if possible, ensuring airlock doors are in place.
Maintaining a sterile environment is recommended for both pre- and post-amplification. Deep cleans should be implemented regularly as a standard procedure within the laboratory and bench tops, pipettes, fridge/freezer handles and containers for consumables should regularly be sterilised before and after PCR using a bleaching agent. Improving pipetting techniques is another factor which can help prevent contamination by ensuring samples are aspirated and dispensed correctly, avoiding uncontrolled samples splashing.
As the use of PCR within HLA typing has become routine, the European Federation for Immunogenetics (EFI) standards suggest wipe tests should be performed every 2 months. We recommend the HISTO SPOT SSP Wipe Test, which has the capacity to detect human genomic DNA and amplificates generated from sequences containing exon 2 and/or exon 3 of HLA A, B, C and exon 2 of the DRB, DQA, DQB, DPA, DPB genes. The test procedure is based on the Sequence Specific Primers (SSP)-PCR. Monitoring can also be performed by running negative controls alongside samples and is another EFI standard - to ensure no false positives are detected from contamination with amplificates (1).





Secure Online Payments
Satisfaction Guarantee
International Service
Premium Customer Service
Inclusive Kits
Customer Chat
Copyright © 2024 MC Diagnostics Ltd.
All Rights Reserved.
Registered in England & Wales
Company Number: 5843597.
Tel: +44 (0)151 2039898
MC Diagnostics Ltd
1 Hawkshead Road
Croft Business Park
Bromborough
Wirral
CH62 3RJ
United Kingdom